Cervical Spine Surgery
Cervical spine surgery may be indicated for:
- Neural decompression
- Spinal stabilization
- Tumour excision
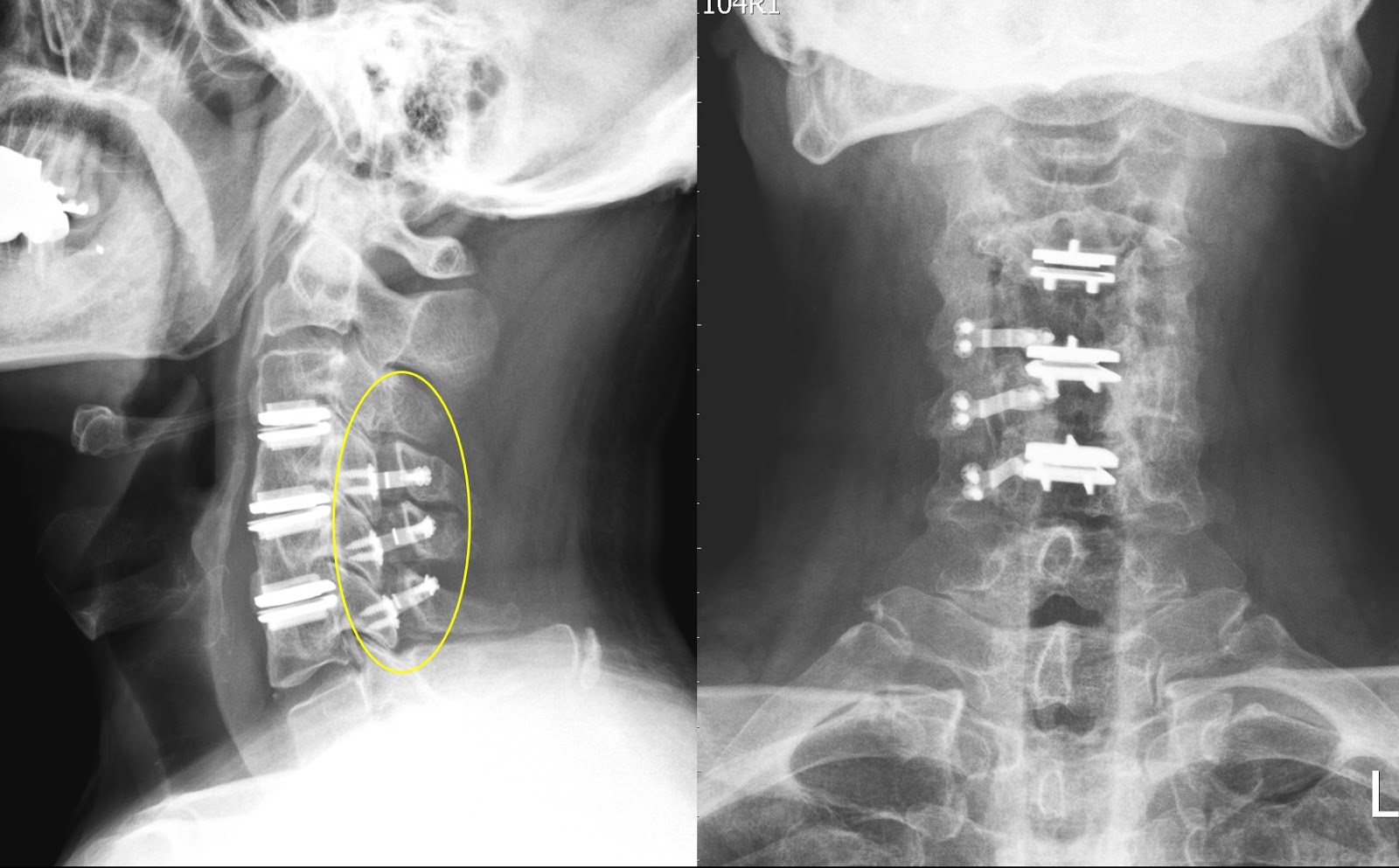
Anterior Cervical Discectomy and Fusion is a common surgical procedure used to treat neck problems such as bulging, herniated disc, degenerative disc disease and spinal instability etc. Discectomy is the removal of the disc and any fragments between the vertebrae. After the disc is removed, the space is filled with a bone graft, the goal is to help the bones to fuse together into one solid bone. This is known as fusion. In order to provide stability during fusion, the doctor may reinforce a metal plate screwed into the vertebrae (cage, screw and plate).The expected outcomes of this operation are to treat for symptoms due to cervical spondylosis aims to relieve pain and prevent further permanent damage to your nerves. Your mobility of neck will be reduced after fixing the disc.
The operation is performed under general anaesthesia. The approach to the cervical spine may vary with individual patient. It can be accessed from the front or from the back. X-ray may be used in the operation room to confirm the level of operation.
Risks and Complications
- Injury
- Larynx , the nerves to the larynx (recurrent laryngeal nerve) causing vocal cord paralysis and a hoarse voice. This is usually temporary.
- Carotid artery, which can cause a stroke resulting in permanent paralysis.
- Spinal cord resulting in temporary or permanent quadriplegia (paralysis of arms and legs).
- Nerve root causing upper limb weakness, sensory loss, or pain temporary or permanent.
- Infection in the wound causing redness, pain and possible discharge or abscess.
- Failure of fusion on the bone.
- Persistent pain
After the patient is awaken from the anesthesia, oral feeding may be started. A normal diet may be resumed as instructed after recovery from anaesthesia. Make sure there is no difficulty in swallowing when resuming normal diet. After general anaesthesia, you may experience discomfort in the throat after tracheal intubation. The side effects of anesthesia including feel tired, drowsy, nausea or vomiting. Inform the nurse if symptoms persist or worsen. You should inform the nurse of wound pain. Proper pain relief treatment by injection or oral medication may be prescribed by the doctor.
Patient would be discharge in 1-2 days when the patient can take oral food and pass urine by himself / herself with health condition.
Advices on Discharge
- Prescription pain medication may be taken as needed.
- Recovery time for the wound generally takes 4 –6 weeks. Recovery of neurological symptoms started before surgery varies, depends on cause and severity of the symptoms.
- You should avoid bending the head forward or backward.
- Do not lift any heavy objects.
- You may gradually return to normal activities. You should avoid sitting for long periods of time, walking is encouraged.
- You usually wear a neck collar in the postoperative period, to hold the neck still in order to let the bone heal and fuse.
- You may shower after discharge unless otherwise instructed. The dressing must be kept clean and dry. The stitches or staples will be removed during subsequent follow-up visit
- You should immediately return to the doctor in the event of severe wound pain associated with redness and swelling, secretion of pus, massive bleeding or high fever over 38°C.
- Any follow-up consultations should be attended as scheduled.
In special patient groups, the actual risk may be different. Other complications may occasionally occur. For further information please contact our spine surgeon.